One of the rare inherited metabolic disorders that we work with is TMAU. It is a disorder that doesn’t cause any physical harm, but causes psychological distress. Over that past few years we have had increasing number of people being referred to our service with suspected TMAU. This is mainly due to increased exposure of the disorder on popular TV programs. I thought I would give you a little insight into what it is and how it is treated.
Table of Contents
What is TMAU?
Trimethylaminuria (TMAU) or Fish Odour Syndrome is a very distressing rare inherited metabolic disorder that causes the sufferer to smell of a variety of malodours including rotting fish, eggs and rubbish. The smell comes from their sweat, breath and urine. Although only recently discovered in the 1970’s, there has been references to it in history, for examples in Shakespeare’s The Tempest, Trinculo talks about a man who smells of a fish! It has been in the spot light more recently after being highlighted on TV programs such as Embarrassing Bodies, The Food Hospital, The One Show and This Morning.
Psychological Effects
Often the person themselves cannot smell it, but other people can, resulting in the person staying away from social situations and can become very withdrawn, lonely and depressed as they are worried about what people will say and think about them.
Causes of TMAU
TMAU is caused by the inability of the person to break down a smelly chemical in the body called Trimethylamine (TMA) into the non-odorous form Trimethylamine oxide (TMAO). The TMA builds up in the body and is excreted via urine and sweat producing the smell.
Treatments for TMAU
Getting diagnosed
Often people have the symptoms for years before getting diagnosed. GP’s have little knowledge of this disorder as it is so rare and it is often the patient that comes up with the diagnosis and then has to persuade the GP to get them tested or to be referred to a specialist centre.Getting referred to a specialist metabolic service is very important to obtain the correct treatment and management. There is information on the internet, but is often factually incorrect or interpreted the wrong way.
Specialist Dietary advice
Many people try to follow the diet without help from a dietitian, they restrict their diet too much, leaving themselves at risk of nutritional deficiencies and weight loss. Our bodies need a minimum amount of choline per day and below this level it is harmful and liver complications can develop. Getting referred to a specialist dietitian for advice is essential so that they can help the person follow a low choline diet that provides adequate amounts of protein, carbohydrates, fats, vitamins and minerals.
Diet for TMAU
The aim of the diet is to reduce the amount of Trimethylamine (TMA) and choline (which is converted by bacteria in the gut to TMA) in the diet.
It is important to eat a wide variety of foods to ensure that the diet provides adequate amounts of essential nutrients and protein. The diet must not be too low in choline as this can lead to liver damage and nutritional deficiencies. Low levels of choline are present in many foods so it is impossible to avoid all dietary choline.
Carbohydrate foods
Most carbohydrate foods are low in choline and can be eaten with each meal as a source of energy. This includes bread, crackers, pasta, rice, potatoes, chips, non-bran cereals, oats. White, brown and whole meal varieties are all low in choline. Bran cereals are higher in choline so you may wish to avoid these.
Protein foods
Protein is needed for growth and repair so protein should be eaten with at least 2 meals per day. Sea fish and crustaceans (crabs, lobster) are high in trimethylamine so should be avoided. Offal (liver, liver pate, kidney, tripe), egg yolks and soybeans very high in choline so should also be avoided. Meat and fresh water fish are good sources of protein and nutrients, sticking to a small to medium sized portions (no bigger than your hand) will ensure the choline content is not too high. Vegetarian sources of protein are lower in choline (i.e. beans, lentils, chick peas, tofu, cheese, egg white, nuts and seeds) so aiming for a mainly vegetarian diet will lower the choline content. Eating meat / fish 2-3 times a week will provide essential nutrients such as vitamin B12, zinc and selenium.
Calcium
Dairy foods (milk, cheese, yoghurt) are a good way to increase the calcium of the diet for bone health, and they are fairly low in choline. 2-3 portions of dairy foods will not increase choline intake greatly. If drinking more milk then nut / rice / coconut milks are a low choline alternative, but need to ensure they are fortified with calcium. It is advised by the government that we get adequate vitamin D for bone health, this can be via sunlight or to take a vitamin D supplement especially in winter.
Fruit and vegetables
All fruit and vegetables are very low in choline so can be eaten without restriction. A group of vegetables called Brassica vegetables are thought to inhibit the enzyme that converts trimethylamine into a none smelly chemical in the liver. These include Brussel sprouts, cauliflower, broccoli and cabbage. This might not be the case for everyone, so check your tolerance to these vegetables.
Food additives
Lecithin, of which choline is a constituent, is a commonly used emulsifier (E322) added to such foods as ice cream, mayonnaise, chocolate and many other manufactured foods.
Some people find foods with large amounts of lecithin exacerbates symptoms so they should try to avoid it. Other people may tolerate it in small amounts therefore tolerance should be tested before avoiding all together.
Vitamins and Minerals
It is important to have a varied diet to ensure adequate intakes of vitamins and minerals. If this can’t be managed then a multivitamin and mineral supplement should be taken, always speak to your dietitian or doctor.
Weight
If you are losing weight unintentionally, then your diet may be too restrictive. Please speak with a specialist dietitian.
How long should the diet for TMAU be followed for?
The diet should be trailed for 3-6 months to see if it helps symptoms. It may not work for everyone and other treatment options can be tried. If it does not help then go back to a normal healthy diet. If the diet is helpful, then to continue and ensure it is adequate by having a review with a specialist dietitian.
The diet is only to control symptoms, so if you are having a quite weekend in then the diet can be relaxed.
Diet Examples
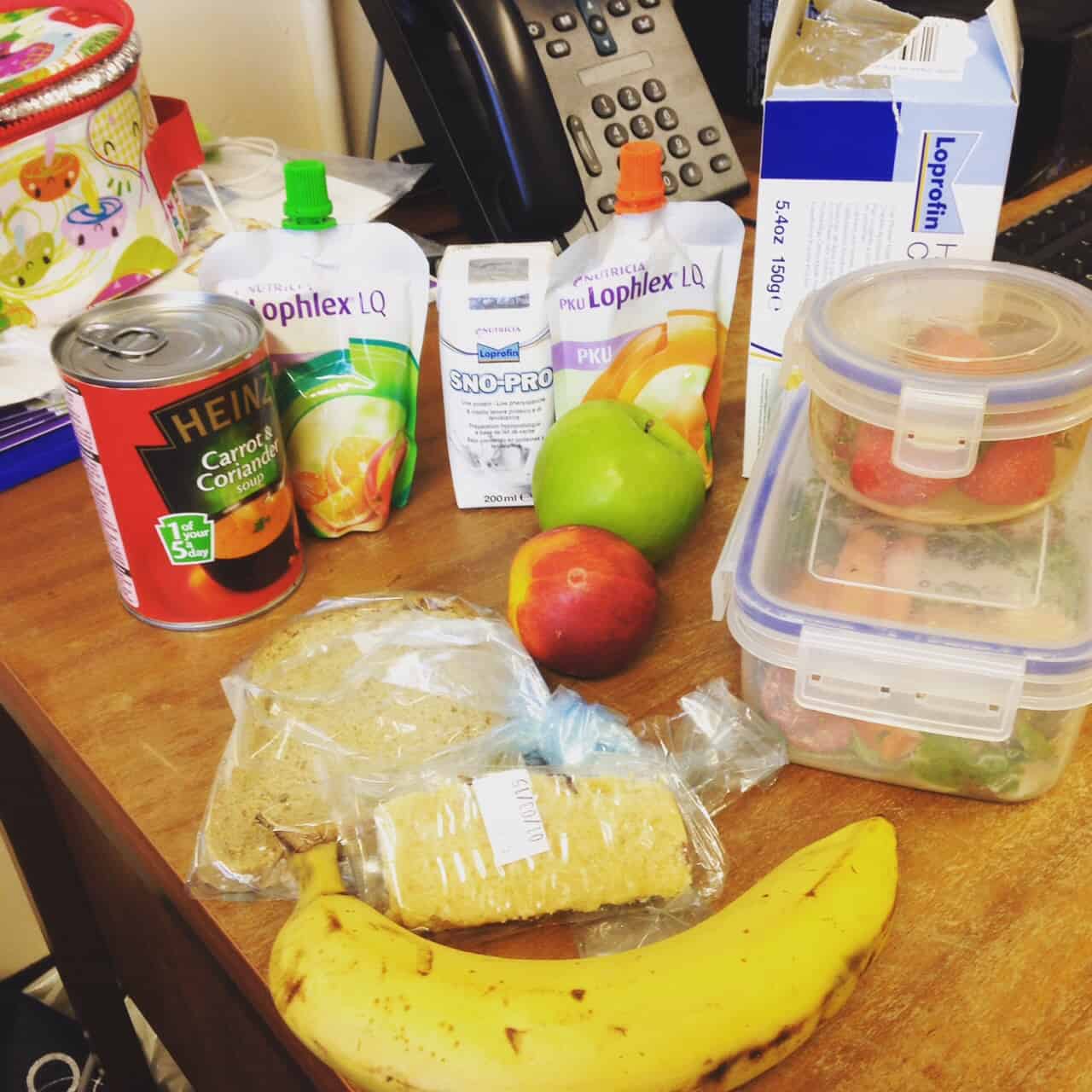
Low choline diet
- Breakfast: cereal and milk, toast x 2 with butter and jam
- Mid am: piece of fruit
- Lunch: cheese salad sandwich with 2 slices of bread, apple, yoghurt and 2 biscuits
- Dinner: small chicken breast, mashed potato, carrots and sweetcorn, stewed fruit and cream
Very low choline diet
- Breakfast: toast x 2 with butter and jam or cereal and rice milk (fortified with calcium)
- Mid am: piece of fruit
- Lunch: cheese salad sandwich with 2 slices of bread, apple, yoghurt and 2 biscuits
- Dinner: kidney bean and vegetable casserole with rice, cake
The above is a guideline, not to replace tailored advice by a specialist dietitian. If you suspect you have TMAU then ask your GP to refer you to a specialist inherited metabolic disorders centre to check the diagnosis is correct before making changes to your diet.
Resources for article
Ellerton C, Chan H, Maritz C. Trimethylaminuria – Fish Odour Syndrome. Complete Nutrition Vol. 10, No.4, August 2010.








Hi Louise, I’m Emma. Do you think there could be a way for doctor’s to make an enzyme fm03 booster/replacement to treat tmau? There seems to be every other enzyme out there. I used to buy an enzyme called protease, it was 50mg, it helped but they stopped selling it, typical. Any other enzymes don’t do the job. Swimming helps with the smell, probably what they use in the pools to keep it bacteria free. I’ve dealt with this over 30 year’s, I’ve asked doc about testing but he looked alien to the concept.
Don’t give up everyone, and don’t worry about what people think too much, stress can make it worse. Look after yourselves and for when you want to pig out on burgers and chocolate then do it once in a while, although I choose to do this at home
Hot lemon water with rosemary and ginger is nice after a cup of coffee. Small pinch of Salt in warm boiled water. Salt scrubs. Flossing every day. I’ve heard black African soap/mud soap is very good d so I’ll be trying that. Drink lots of water, supplements, Berries I find help too. I make a joke out of myself when I know I smell, it makes people laugh and hopefully they’d understand a bit more too, if they don’t then whatever, live your life ❤️
Hi,
I haven’t seen my GP yet about this condition (I’m a teen, currently working up the courage to ask my mum)
however i’ve noticed a symptom.
My body odor smells fishy/vinegary.
In class, a friend said “it smells sour” from where I was standing however I smelt myself briefly and I couldn’t smell anything
My breath also smells different to what it smelt before (it may be the cause of the toothpaste I’m using, not sure)
It’s currently the summer holidays so I sit by the stairs hoping to cool down and my odor just stinks up the hallway in seconds
After I shower, I could still smell my body odor
Not sure what to do, help?
Hi, thanks for asking. I know it is really hard to talk about to parents and Gp, but it is so important to go to your GP to check there is nothing else that is causing the body odour first. They maybe an easy treatment for it. If they can’t find anything else to cause it then then you can be investigated for TMAU. You could then be referred to a specialist centre. Take care, Louise
Thank you!
Also another question
Will other people be able to smell the odor if they sit next to me + does spraying antiperspirant deodorant on the armpits help the fishy odor?
Hi
I think I have TMAU. But I haven’t been diagnosed yet.
The smell is so irritation that I feels like my nose would burn .
Please advise me what shall I do?
Hi, speak to your GP / doctor about it. See if they can refer you to a specialist centre (Inherited Metabolic Disorders).
Your diet for individuals with TMAU can be very helpful . Thank you for posting it. I took your post and sent it to MEBO on Facebook that is an organization for people US and international countries that suffer TMAU 1 and TMAU 2.
Thank you
Your welcome. The founder was very impressed with your nutrition and she is an expert in food nutrition since she found what foods to consume. She suffers from TMAU type2.
We love this post! Thank you for bringing awareness to the TMAU community and providing healthy approaches to help alleviate symptoms. If anyone would like more information about TMAU, the nonprofit I work for is starting clinical trials for non-prescription over the counter supplement and we’d love to hear from you.
Dermetel.org
https://givebutter.com/dermetel-trials
Hi – I have had the tmau gentic test taken and I am still waiting for the results – but the low choline diet has improved my symptoms greatly.
To begin with I think I was far too restrictive with my diet and I have developed a condition called arcus senilis caused by high cholesterol – I am having a blood test next week and my gp has hinted at statins. My diet is pretty much low in everything including choline,fat ,salt and sugar – I don’t drink or smoke and lead an active lifestyle so wondered if my diet could be having a knock on effect to my bodies fat metabolism?
thank you for your message. I can’t answer your query, best to talk to your dietitian who can look over your medical history and clinical picture to go with it. Louise
Hi, do you have any recommendations for a good low-protein recipe cookbook?
Hi, I wouldn’t recommend a low protein diet for TMAU, but if you want to reduce the protein in your diet, but still get adequate then a vegetarian / vegan diet (ensuing nutritionally adequate) would be the best.
Hi Louise
My husband has TMAU (undiagnosed but suffered since he was 14 years old.
I am trying to help compile a food list but we are getting conflicting information and so I wondered do you have an updated food list? He is currently fasting and o lay eating one meal per day due to the effects thisnis having on him. Pls help 🙂
Hi Lindsey, I am sorry to hear this. I would suggest he needs a referral to a specialist inherited metabolic disorders centre who will have a dietitian who can provide info. He is at risk of weight loss and nutritional deficiencies. Louise
Hello,
Do you know if oatmeal will be good to eat with tmau?
Hi, yes oatmeal is fine. Louise
Hi Lindsey – I also suffer from tmau -has your husband looked at the tmau community on rare connect – its a forum for people suffering from the same conditions,and there is a lot of useful advice about diet and supplements from other tmau members
Sarah
Hello Ms Robertson, I for sure have Tmau
I just bought a vegan-smart plant based protein pouder which is egg, soy and gluten free !, doesn’t contain any artificial flavours.
BUT, the only one i could get is a vanilla flavour one. Now that i have it, i can notice it has quite a strong vanilla smell, i can’t help but being terorized by the possibility that it could make things worse.
Should i still use it ?
I wonder: if a food has a strong smell, would it necessarly mean it”ll worsen the smell ?
thank you in advance
Hi Jake,
the vegan protein powder sounds suitable to use. It is not to do with the food smell. Only if the food contains a large amount of choline (high source = egg and soy beans) or TMA (found in sea fish) then to avoid. Best wishes, Louise
Hello I’m a Colombian guy struggling possible TMAU, and I’m on a vegan diet. I’ve been eating lots of leafy vegetables, are they ok? And I wanted to ask you if mushroom and spirulina could be ok?
Hi Mateo, A vegan diet will be lower choline diet so good for TMAU, yes green leafy veg and mushrooms fine. Spirulina fine in small amounts. Ensure adequate protein sauces from plant-based foods. Louise
I hav’nt been diagnosed with TMAU but no doubt have probably got it. Everything I have read about it suggests this. I am at a loss as what to do and am not enthusiastic about going to my doctor. I asked my doctor a few year ago to help me. He thought I was being silly for want of a better word but arranged for me to see a doctor at the hospital who after seeing me suggested it could be down to stress I was going through at the time. He obviously was’nt clued up on TMAU and that was the end of it until now. I was lucky enough to find out about it through the internet. I could do with some help as I am desperately down with this malady,please someone help me. Ed Elliott.
Hi Ed, sorry to hear this. Are you in the UK? ask your GP to refer you to a centre that specialises in Inherited Metabolic Disorders as these teams know about TMAU and will be able to help you. If you are feeling down see if you can access some counselling (can ask via your GP surgery). Best wishes.
I am in Kansas City. I believe that I have this condition. Over the last 4 yrs, everything keeps pointing back to TMAU. I cannot convince my Dr to do Genetic testing. Do you know any Dr’s that work with this type of condition in the Kansas City metro area? Kansas would be okay too. I am crying out for help. So embarrassing, I am to the point of isolation.
Thank you for everything
Sherry
Hi Sherry, I am sorry to hear this. I am in the UK so I don’t have contacts in the US. We use a urine test for TMAU in the UK rather than genetic testing. A lot of people suffer from secondary TMAU which is not caused by a genetic defect but bacterial overgrowth. Try asking your Dr to have a look into if anyone specialises in it locally. Good luck.
Hi Sherry, I am also in KC and looking into TMAU. I wonder if Louise can help us swap email addresses?
Rachel
Hi Louise
I have been tested for the TMAU, I have primary TMAU.
I wanted to understand something.
Should we only reduce choline intake, or are there other precursors to reduce intake?
As for the amount of protein, can I take rice protein powder?
Does the amount of protein we take affect the bad smell?
What supplements could I take and how to reduce the odor?
Do sports and sweating help or make the situation worse?
Hi, I’ll just briefly comment as hard to give advice without knowing your situation. Yes, choline is found in protein, so not to overeat protein, a vegetarian diet (using plant-based protein sources) will be lower in choline than animal sources. You must still get adequate protein in your diet for health. It is the accumulation of TMA (gut bacteria turns choline into TMA) that causes the smell. Potentially sweating could make the odour more pronounced as the TMA is excreted in body fluids. I would advise you to see a specialist to discuss in detail.
So in addition to the choline, we must also reduce the amount of protein?
Currently I follow a vegetarian diet made by a nutritionist who follows me regarding TMAU.
I just wanted to be sure if the amount of protein taken in affected the smell.
Let’s say that the bad smell is as if it came from under the skin, often I can not understand well where it comes from, but if it’s windy it feels a lot more, is it normal?
So I’m doing well to follow the vegetarian diet, more than anything else is based on the cheese we say.
Do you recommend the supplements to be taken to ensure that the odor drops?
And can you tell me if you take it before or after meals?
Thanks a lot in advance, I ask you these questions because in Italy you know very little about the treatment of this disease.
Hi Louise
I read somewhere that if you have tmau you should eat raw fruits and vegetables and drink origanum tea is this true?
Hi, no if you only ate this your diet would be deficient. Follow the guidelines in the post above.
I thought beans were high in choline. Are there certain beans to stay away from?
Hi Sandra, beans do have choline in, but compared to meat, they have less per portion. We can’t say for sure which beans are better than others for choline as we don’t analyse the choline in foods in the UK. As you can’t have a choline-free diet and you need protein in your diet then an option of beans, pulses of lentils are good options and lower choline options than meat.
Dear Ms. Robertson,
Are sunflower lecithin 1200 mg softgels safe to ingest as a supplement everyday or does it raise trimethylamine levels and TMAO levels in the body?
Thank you very much.
Best regards.
Randy
Hi, if you have been diagnosed with TMAU then these supplements could increase your TMA levels as choline is contained in lecithin.